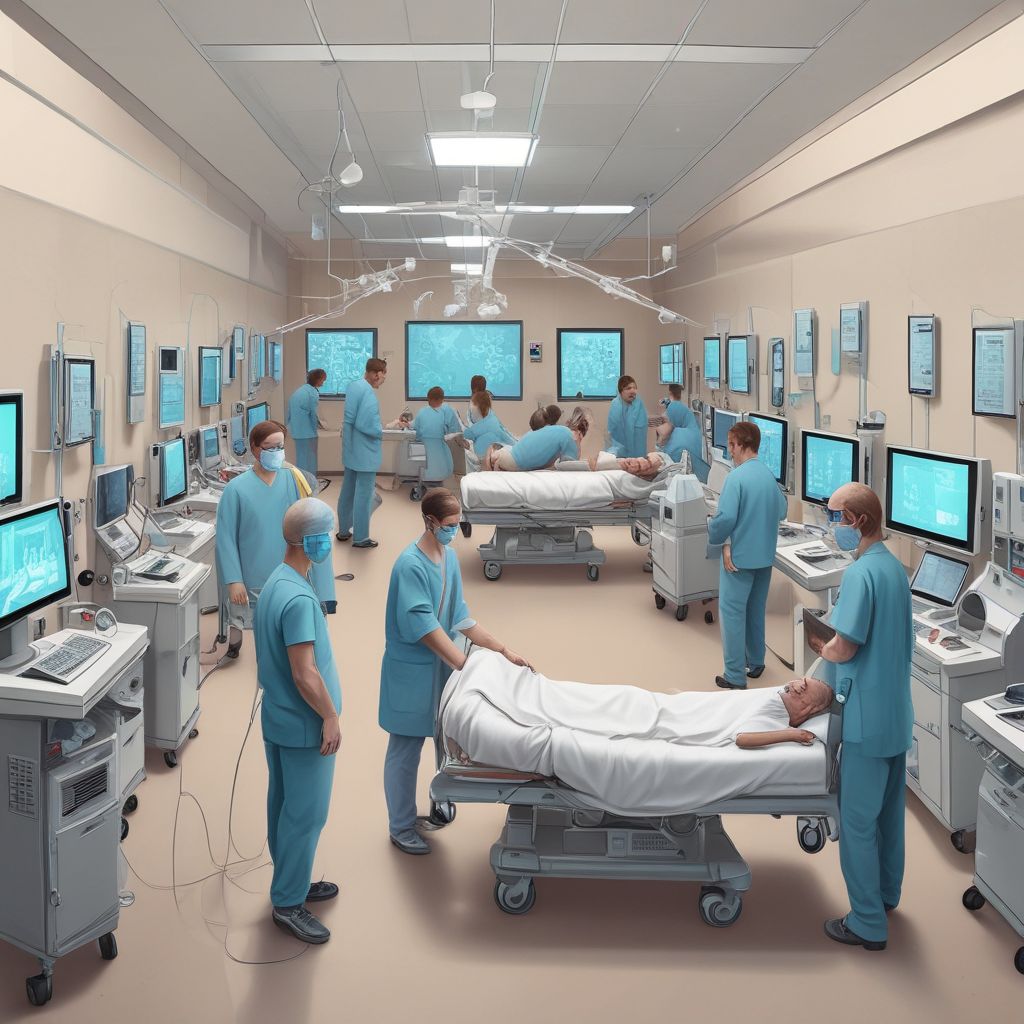
The rise of Digital-Twin ICUs is reshaping how hospitals manage capacity and respond to crises: by creating live, data-driven simulations of patient flow, staffing, and resource use, clinical teams can predict bottlenecks, test interventions, and prevent dangerous overcrowding before it happens.
What is a Digital-Twin ICU?
A Digital-Twin ICU is a virtual replica of a real intensive care unit that mirrors the current state of patients, staff, beds, equipment, and workflows in real time. It ingests streams of data from electronic health records (EHRs), bed management systems, ventilators, IoT sensors, and staff scheduling tools to run continuous simulations that forecast near-term demand and test operational decisions without affecting patient care.
Core components
- Real-time data integration: Patient vitals, admissions/discharges, lab results, and device telemetry feed the model continuously.
- Process and agent-based models: Algorithms represent patients, staff, beds, and equipment as interacting agents to simulate flow and outcomes.
- Simulation engine and analytics: What-if engines run scenarios (e.g., sudden influx, staff shortage) and calculate key performance indicators like wait times and ICU occupancy.
- Dashboard and alerting: Clinicians and operations staff receive clear visualizations and actionable recommendations through dashboards and automated alerts.
How Digital-Twin ICUs prevent overcrowding
Overcrowding in critical care escalates risk and degrades outcomes; Digital-Twin ICUs tackle this by turning uncertainty into foresight.
- Short-term forecasting: Predicting occupancy over the next 6–72 hours lets administrators arrange transfers, delay elective surgeries, or open surge capacity proactively.
- Prioritization and triage testing: Simulation allows testing triage policies and transfer criteria on virtual patients to understand their downstream effects before applying them in reality.
- Resource reallocation: The twin can suggest reassigning ventilators or relocating specialized staff to anticipated hotspots, minimizing response lag.
- Queue management: It models waiting times for procedures and consults, enabling preemptive scheduling changes that flatten visible and hidden queues.
Example scenario: Influenza surge
When a regional influenza wave begins, a Digital-Twin ICU can combine community case data with current admissions to simulate multiple surge scenarios. Hospital ops can evaluate whether adding a temporary step-down ward, reassigning anesthesia staff, or accelerating discharges from the step-down units will keep ICU occupancy below critical thresholds, and pick the least disruptive option with simulated outcomes attached.
Optimizing staffing and workflows
Staffing is one of the most complex operational variables in an ICU. Digital twins translate staff schedules, competencies, and fatigue models into predictions of care capacity.
- Skill matching: The model identifies mismatches between patient acuity and available competencies and suggests cross-training or shift swaps to close gaps.
- Fatigue-aware rostering: By simulating workload across shifts, digital twins can propose rosters that reduce burnout risk while maintaining coverage.
- Process redesign testing: Proposed workflow changes—such as modified rounds, dedicated float teams, or mobile critical care outreach—can be trialed in the simulation to quantify expected improvements.
Running crisis drills without risk
Beyond daily ops, Digital-Twin ICUs support preparedness by running realistic crisis drills—mass casualty events, power outages, or pandemic spikes—within the virtual environment.
- Low-cost, repeatable drills: Teams can iterate multiple response strategies and measure KPIs like time-to-first-intake, mortality risk, and equipment strain without exposing patients.
- Cross-department coordination: The twin can include upstream ED flows and downstream step-down units so that drills reveal systemic bottlenecks, not just ICU-level problems.
- After-action learning: Each simulated drill produces a quantitative after-action report that helps refine protocols, checklists, and communication trees.
Real-world impact and evidence
Early adopters report measurable benefits: reduced peak occupancy, fewer emergency transfers, improved staffing efficiency, and faster response times to surges. A community hospital network that implemented a digital twin reported a 15% reduction in ICU boarding time and avoided the need to open an emergency surge ward on two high-demand days.
Key metrics to track
- ICU occupancy and projected occupancy
- Time-to-bed for incoming critical patients
- Staffing shortfall hours
- Equipment utilization (ventilators, dialysis machines)
- Simulated vs. actual outcomes after implemented interventions
Challenges and considerations
Implementing a Digital-Twin ICU requires careful attention to data quality, privacy, and clinician trust.
- Data integration complexity: EHRs, device telemetry, and scheduling systems often use different formats; robust ETL and interoperability standards are essential.
- Model transparency: Clinicians must understand model assumptions and confidence bounds to trust recommendations; explainable analytics and human-in-the-loop governance help.
- Security and ethics: Strong data governance and privacy-preserving techniques (de-identification, access controls) are required to protect patient information.
- Change management: Adoption succeeds when simulations complement—not replace—clinical judgment and when frontline staff participate in model design and validation.
What the future holds
As sensor networks and real-time analytics improve, Digital-Twin ICUs will become more granular—modeling organ support trajectories, predicting deterioration hours earlier, and integrating community health data for regional coordination. Advances in federated learning will also enable sharing model improvements across hospitals without exposing raw patient data, accelerating collective preparedness.
Getting started: a pragmatic roadmap
- Start small: pilot on a single ICU unit with clear outcome goals (reduce boarding time, improve staffing utilization).
- Prioritize data sources: connect EHR admissions, bed management, and staff scheduling first to unlock immediate value.
- Engage clinicians: form a cross-functional steering group to set scenarios, validate outputs, and refine alerts.
- Iterate and scale: use pilot results to expand coverage across units and integrate more data feeds (device telemetry, lab pipelines).
Digital-Twin ICUs convert reactive firefighting into proactive, measured operations, giving hospitals the ability to avoid overcrowding, deploy staff more effectively, and rehearse crises without risk. By combining clinical expertise with real-time simulation, hospitals can protect patient safety while optimizing limited resources.
Conclusion: Embracing Digital-Twin ICUs equips health systems with a predictive mirror of their critical care capacity—helping teams act early, allocate smarter, and save lives.
Ready to explore a Digital-Twin ICU pilot at your facility? Contact your hospital operations or digital health team to begin a discovery workshop today.