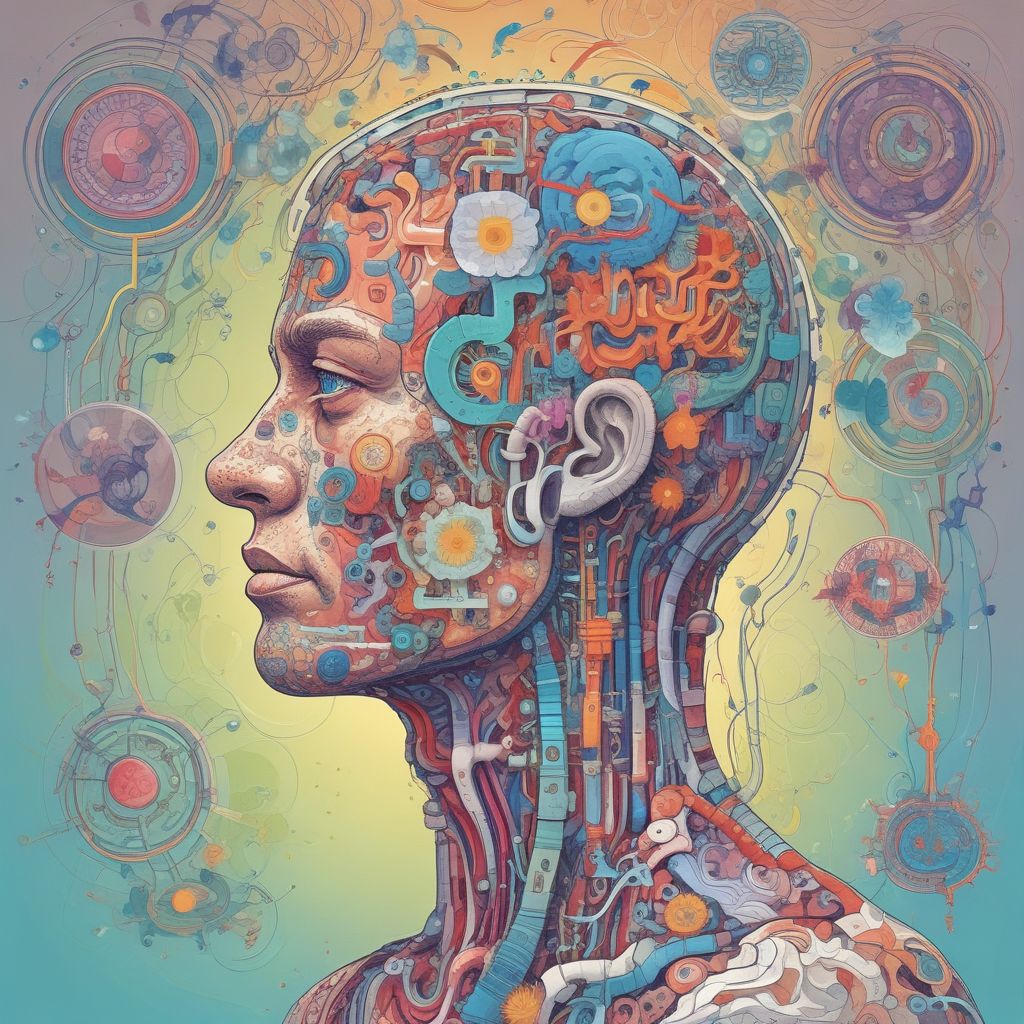
The Hidden Dialogue Between Gut and Brain
For decades, scientists have known that the gut and brain share a complex communication network. This “gut-brain axis” involves neural pathways, hormonal signals, and immune responses. Recent research reveals that trillions of gut bacteria actively participate in this dialogue through chemical signals and electrical impulses.
These microorganisms produce neurotransmitters like serotonin and GABA, influence inflammation levels, and even modify the brain’s blood barrier. Dysbiosis — an imbalance in gut flora — has been linked to depression, anxiety, and neurodegenerative diseases. The challenge has always been decoding these microbial “languages.”
Machine Learning Breaks the Code
Advanced machine learning algorithms now allow scientists to analyze vast datasets of microbial activity. By processing metadata from metagenomic sequencing, metabolomic profiles, and electrophysiological recordings, AI identifies patterns invisible to human researchers.
One breakthrough came from a 2023 study at Stanford University. Researchers trained a neural network to correlate specific bacterial gene expression patterns with brain scan data. The system learned to predict anxiety levels with 89% accuracy based on gut microbiome composition alone.
Key Discovery: Signal Patterns
The AI revealed that bacterial communities don’t simply produce chemicals — they send synchronized signals. These patterns include:
-
Timed release of short-chain fatty acids that modulate brain inflammation
-
Electrical impulse sequences resembling neural activity
-
Biofilm formations that act as “antennas” for signal transmission
From Discovery to Treatment
This understanding opens doors for bacterial-based therapies. Unlike traditional psychiatric medications that target human cells, these approaches modify gut microbes to influence mental health indirectly.
Current Clinical Approaches
Early-stage trials are testing several strategies:
-
Specially engineered probiotics that deliver calming signals during stress
-
Prebiotic diets customized to boost beneficial bacterial networks
-
Vagus nerve stimulation paired with microbial signal amplification
In one pilot study, participants receiving a multi-strain probiotic formulation showed a 40% reduction in PTSD symptoms after three months. The treatment focused on enhancing Lactobacillus and Bifidobacterium populations that produce gamma-aminobutyric acid (GABA).
Personalized Psychiatric Medicine
Machine learning enables truly personalized treatments. AI models now analyze an individual’s unique microbiome to create tailored therapeutic plans.
A Berlin-based startup uses algorithmic profiling to match patients with specific bacterial consortia. The process begins with a stool sample and brain imaging session. Data feeds into an AI that recommends:
-
Targeted probiotic blends
-
Diet modifications to support beneficial strains
-
Timing for therapeutic interventions based on circadian rhythms
Challenges on the Path Forward
Despite promising results, significant hurdles remain. Microbial ecosystems are incredibly complex and vary widely between individuals. Reproducing lab findings in diverse populations requires rigorous standardization.
Ethical questions also arise. Modifying gut bacteria raises concerns about long-term effects and informed consent. Regulatory frameworks struggle to keep pace with rapidly evolving microbiome therapies.
Key Challenges Include
-
Maintaining bacterial viability during storage and delivery
-
Understanding indirect effects on the immune system
-
Long-term safety monitoring across different age groups
The Future of Microbial Psychiatry
Researchers envision a future where mental health assessments include routine microbiome analysis. AI-driven platforms could predict psychological crises by monitoring shifts in gut bacterial activity.
Potential applications extend beyond traditional psychiatric disorders. Studies suggest microbial therapies might aid recovery from Alzheimer’s disease by reducing neuroinflammation. Other investigations explore combinations with existing treatments — for example, pairing antidepressants with synbiotic formulations that enhance drug efficacy.
A New Era of Holistic Health
The convergence of artificial intelligence and microbiology marks a paradigm shift in understanding mental health. By decoding the gut microbiome’s hidden languages, scientists are opening pathways to treatments that work with the body’s natural systems rather than against them.
As technology advances, these bacterial-based therapies could become as common as vitamin supplements — offering precise, personalized support for mental well-being through the power of our internal ecosystems.