What Are Swallowable Sensors?
Swallowable sensors resemble large vitamin pills, about the size of a pain reliever. Encased in biocompatible materials, they contain microelectronics, batteries, and chemical detectors. Once swallowed, they navigate the stomach, small intestine, and colon over 24-48 hours.
Powered by tiny batteries or stomach acid, these capsules transmit data wirelessly to a wearable patch or smartphone app. No wires, no surgery—just swallow and monitor. Early prototypes date back to the 1970s, but advances in nanotechnology have made them precise and affordable.
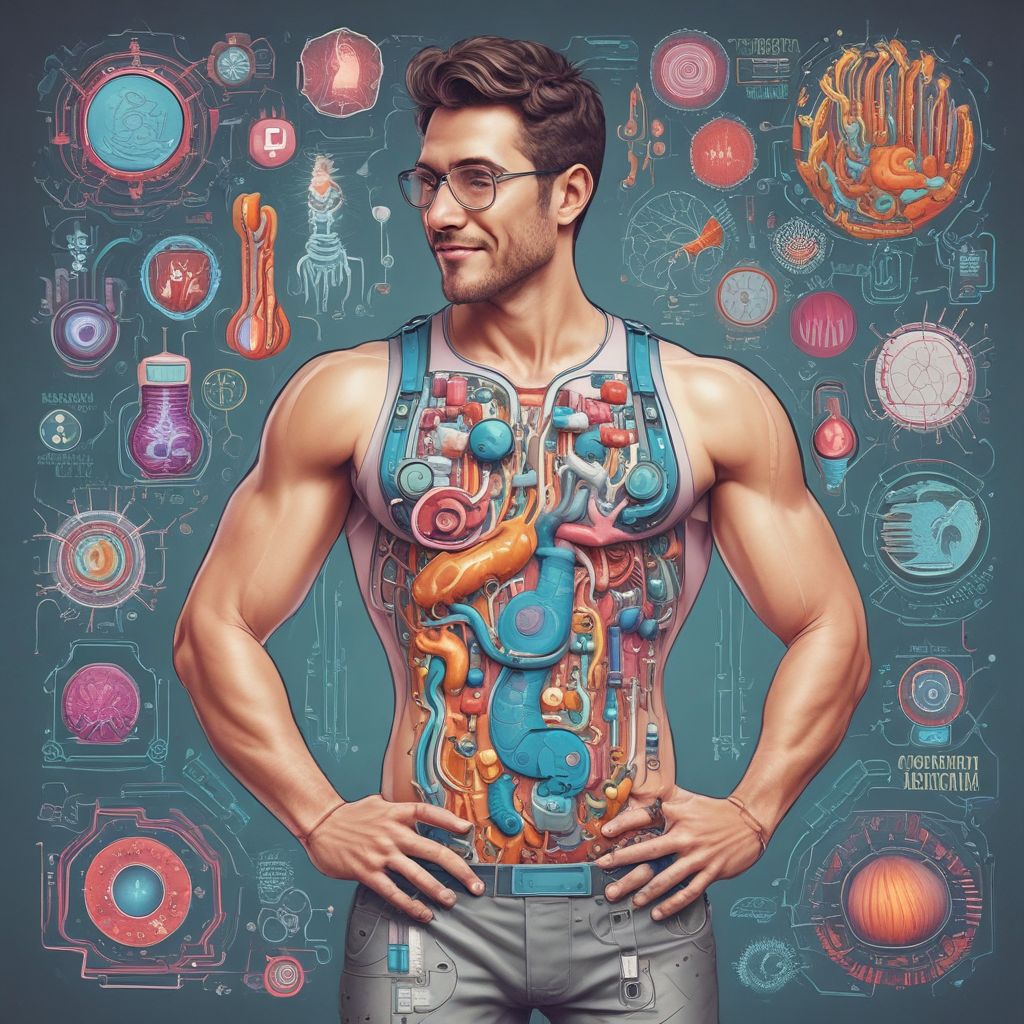
Key Components Inside the Capsule
- Sensors: Detect pH levels, temperature, oxygen, and microbial gases like hydrogen and methane.
- Transmitter: Bluetooth or radiofrequency for real-time data streaming.
- Power Source: Dissolvable batteries or inductive charging via external devices.
- Shell: Edible polymers that dissolve post-mission or pass naturally.
Companies like EnteroSense and research labs at MIT are pushing boundaries, with clinical trials showing over 95% data accuracy.
How They Track Microbiome Health in Real-Time
The gut microbiome—your personal bacterial community—produces unique signatures during digestion. Sensors capture these by measuring volatile organic compounds (VOCs) and short-chain fatty acids (SCFAs), key microbiome byproducts.
For instance, high hydrogen levels might signal small intestinal bacterial overgrowth (SIBO), while elevated SCFAs indicate healthy fermentation. Data streams continuously, creating a “gut diary” that apps visualize as graphs and heatmaps.
Unlike blood tests, which lag by hours, these sensors provide minute-by-minute insights. This granularity reveals how foods trigger microbial shifts, linking diet to health outcomes.
Real-Time Data Flow
- Swallow capsule with water.
- Sensor activates in stomach, begins logging.
- Data beams to abdominal patch every 30 seconds.
- App processes info using AI algorithms for patterns.
- Results sync to cloud for doctor review.
Analyzing Digestion and Inflammation
Digestion tracking starts with pH mapping. The stomach is acidic (pH 1-3), duodenum neutralizes to 6-7, and colon varies. Deviations signal issues like acid reflux or poor motility.
Inflammation detection focuses on biomarkers like calprotectin or cytokines, sensed via electrochemical reactions. Sensors use nanotechnology—gold nanowires or graphene—to detect femtogram levels, far surpassing lab tests.
One study from Caltech’s ingestible device spotted GI bleeding via color-changing dyes, alerting users instantly. For chronic conditions like IBS or Crohn’s, this means early intervention before symptoms flare.
Combining metrics paints a full picture: slow transit plus high inflammation suggests dysbiosis, prompting targeted fixes.
Personalized Nutrition Advice from Gut Data
The magic happens in AI-driven analysis. Apps like those from Viome or emerging sensor platforms cross-reference your data with vast databases of 1,000+ foods and microbiomes.
If sensors detect low butyrate (an SCFA for gut lining), the app recommends fiber-rich foods like oats or inulin supplements. Methane dominance? Cut fermentable carbs to starve methanogens.
Sample Personalized Plans
- High Inflammation Profile: Anti-inflammatory diet—omega-3s from salmon, turmeric, avoid processed sugars.
- Poor Digestion: Prokinetic foods like ginger; probiotics tailored to detected strains.
- Healthy Baseline: Maintain diversity with fermented foods, prebiotics.
- Microbiome Imbalance: Phage therapy or specific-strain yogurts.
Users report 30-50% symptom improvement in trials. Integration with wearables like Oura or Whoop adds context, factoring sleep and activity.
Current Technologies and Pioneers
Medtronic’s PillCam leads visuals but lacks biosensors. Next-gen: Motus GI’s Pure-Vu for cleansing, but true sensors shine in research.
Proteus Biomedical’s digital pills (RIP’d but influential) verified medication adherence via stomach signals. Today, Carnegie Mellon’s “O robo-pill” unfolds like origami to sample tissues.
Commercial frontrunners include:
- EnteraSense: HSE Ireland-backed, FDA-cleared for motility.
- MC10/Anzu: Stretchable electronics for multi-parameter tracking.
- UCSD’s Nano-Sensors: Detect viruses and bacteria in trials.
Costs hover at $200-500 per use, dropping with scale. Insurance covers for IBD patients in pilots.
Benefits of Ingestible Gut Tech
This tech empowers proactive health management. Key advantages include:
- Non-Invasive: No endoscopy prep or radiation.
- Precision: Pinpoints issues by GI segment.
- Actionable Insights: Daily nutrition tweaks beat vague advice.
- Remote Monitoring: Ideal for telemedicine.
- Research Goldmine: Anonymized data accelerates science.
Athletes use it for performance fueling, while seniors monitor for malnutrition risks.
Challenges and the Road Ahead
Hurdles remain: Battery life limits to 72 hours max. Data overload requires smarter AI to avoid alert fatigue. Regulatory approval lags for full microbiome panels.
Privacy concerns loom—gut data is intimate. Blockchain-secured apps address this, ensuring user control.
Future visions: Multi-day capsules, self-dissolving swarms, gene-editing payloads for dysbiosis. By 2030, expect grocery apps suggesting meals based on your last swallow.
Getting Started with Gut Sensors
Consult a gastroenterologist for IBS or unexplained bloating. At-home kits launch soon via subscription, like continuous glucose monitors.
Pair with journaling: Log meals alongside sensor data for best results. Early adopters rave about resolving lifelong issues.
In summary, swallowable sensors turn the gut from black box to open book. By decoding microbiome whispers in real-time, they usher in an era of hyper-personalized nutrition. Your optimal diet might be one pill away.
(Word count: 1,128)