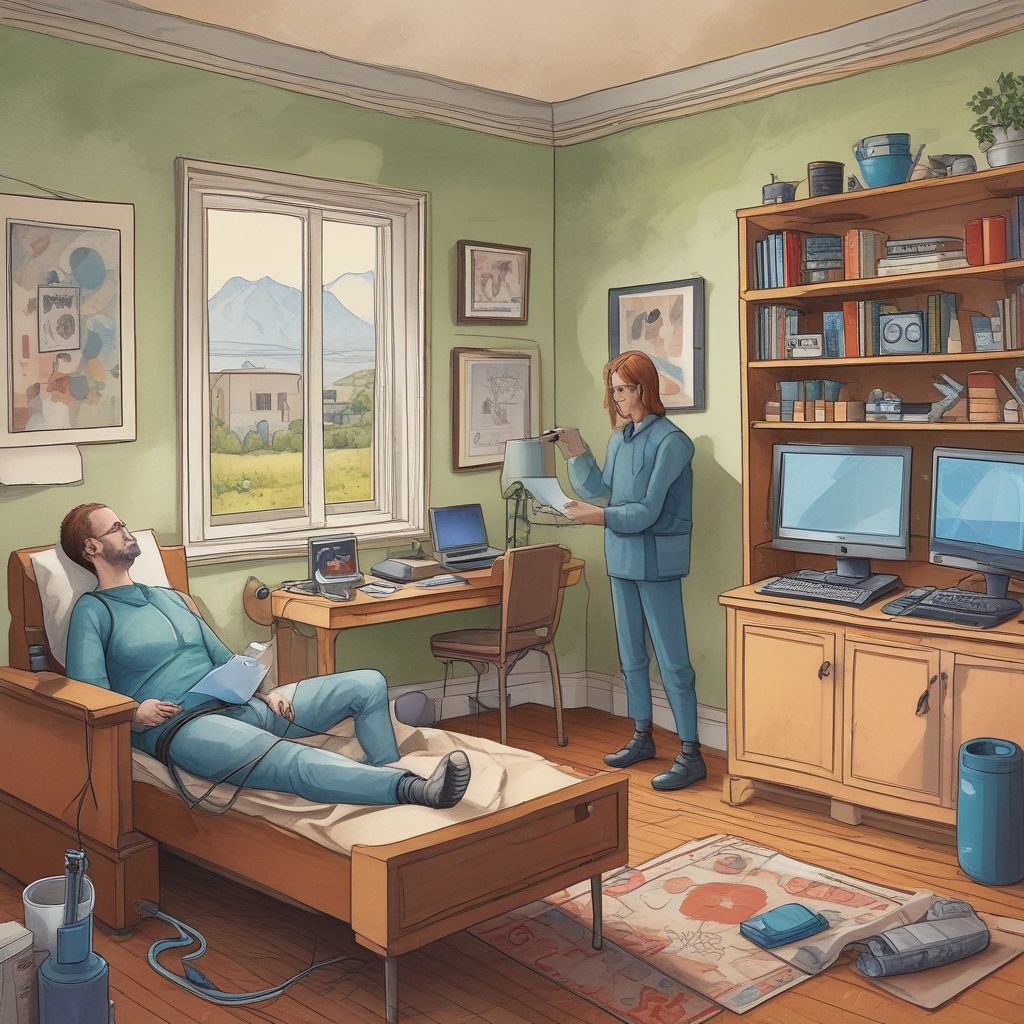
Ambient Telehealth is reshaping chronic care by turning homes into continuous, clinically useful data sources using unobtrusive passive sensors and voice biomarkers. Providers and caregivers can detect subtle changes in behavior, mobility, sleep, and speech that precede deterioration—enabling early intervention, lowering emergency visits, and reducing hospitalizations while preserving patient privacy. This article explains how the technology works, why privacy-first design matters, and practical steps for integrating ambient monitoring into remote chronic care programs.
What is Ambient Telehealth?
Ambient Telehealth refers to non-wearable, in-home monitoring systems that collect data passively—without active input from the person being monitored—to support health decision-making. Rather than relying solely on episodic clinic visits or patient-initiated reports, ambient solutions continuously gather contextual signals (movement, appliance use, ambient sound patterns, and more) and extract clinically meaningful features like activity levels, sleep fragmentation, and conversational markers from voice.
Passive Home Sensors: The silent clinicians
Passive technologies include motion detectors, door sensors, pressure mats, smart plugs, bed sensors, and environmental monitors (temperature, humidity, air quality). These devices detect patterns such as:
- Daily routine changes (missed meals, fewer outings)
- Declines in mobility (slower walking speed, more time seated)
- Sleep disruptions (frequent night awakenings, restless bed activity)
- Medication non-adherence signals (unopened cabinets or smart pill bottle events)
Because they don’t require charging or wearable compliance, passive sensors are especially suitable for older adults and people with cognitive or mobility limitations.
Voice Biomarkers: Listening for clinical signals
Voice biomarkers analyze speech characteristics—tone, pace, articulation, pause patterns, and respiratory markers—to surface signs of disease progression or acute change. Research links voice features to conditions such as heart failure (breathless speech), Parkinson’s disease (reduced prosody), depression (monotone, longer pauses), and respiratory infection (cough patterns). When analyzed longitudinally, small changes in voice can flag deterioration earlier than self-reported symptoms.
Why Privacy-First Matters
Ambient monitoring raises legitimate privacy concerns because it operates inside personal living spaces. Privacy-first design protects dignity and encourages adoption while still delivering clinical value. Key principles include:
- Data minimization: collect only signals required to answer clinical questions.
- Edge processing: analyze raw audio or video locally and transmit only extracted features or alerts.
- Encryption & access controls: secure data at rest and in transit and limit access to authorized care teams.
- Transparent consent: explain what is collected, how it’s used, and how long it’s retained.
- Configurable fidelity: allow residents to mute microphones or define sensitive zones/times.
Clinical Value: Early Intervention and Reduced Hospitalizations
Ambient Telehealth can change the trajectory of chronic illness management by shifting care from reactive to proactive. Examples of clinical impact include:
- Early detection of heart failure exacerbations through reduced activity and nocturnal restlessness, enabling diuretic adjustments before admission is needed.
- Preventing falls by identifying gait slowdowns and home hazards via motion pattern analysis and alerting caregivers to intervene.
- Managing COPD and respiratory illnesses by recognizing increased cough frequency or breathlessness in speech and triggering remote assessments.
- Monitoring medication routines and social withdrawal in people with dementia to prevent complications and unsafe wandering.
Multiple pilot studies and emerging real-world deployments show reductions in emergency department visits and shorter inpatient stays when ambient systems are paired with timely clinical workflows.
Implementation Best Practices for Providers
Successful ambient telehealth programs combine technology, clinical pathways, and human-centered workflows:
- Define clinical goals: target specific outcomes (e.g., reduce CHF admissions) and choose sensor types that map to those goals.
- Integrate with EHR and care teams: send prioritized alerts to clinicians and pair them with nursing follow-up protocols.
- Use layered risk models: combine sensor signals with medical history and patient-reported data to reduce false positives.
- Train staff: teach clinicians how to interpret sensor-derived metrics and how to translate alerts into interventions.
- Pilot, measure, iterate: start with focused cohorts, track outcomes (hospitalizations, cost, adherence), and refine algorithms and workflows.
Addressing Challenges and Ethical Considerations
Several barriers must be managed for scalable, ethical deployments:
- False positives/alert fatigue: implement threshold tuning, human review, and context-aware filtering to keep alerts actionable.
- Equity and access: ensure solutions work in low-bandwidth homes and with diverse voices and living arrangements.
- Regulatory compliance: align with HIPAA, GDPR, and local medical device rules; document risk assessments and validation studies.
- User trust: co-design with patients and caregivers to ensure cultural sensitivity and address surveillance fears.
Privacy-First Technical Patterns
Concrete technical approaches that preserve privacy while enabling clinical insights:
- Edge-first pipelines: process audio for voice biomarkers on a local hub and transmit only numerical features or alarms.
- Federated learning: improve models across homes without sharing raw data.
- Time-limited storage and audit logs: auto-delete raw inputs after processing and provide audit trails for data access.
- Consent dashboards: let users review data summaries, pause monitoring, and control sharing with family or clinicians.
Looking Ahead: Scalable Care Without Sacrificing Dignity
Ambient Telehealth promises a future where chronic care becomes anticipatory rather than punitive—where declining health markers prompt compassionate, timely support instead of preventable crises. As sensor fidelity improves and voice biomarkers mature, the combination of privacy-first engineering and clinically focused workflows will be essential to realize lasting reductions in hospitalizations and better quality of life for patients living at home.
Conclusion: Ambient Telehealth, powered by passive home sensors and voice biomarkers, offers a pragmatic path to earlier intervention and fewer hospital stays—if privacy and clinical integration remain central to design. Start with clear clinical goals, prioritize privacy-by-design, and measure outcomes to build trust and demonstrate value.
Ready to explore a privacy-first ambient monitoring pilot for your practice or care network? Contact a telehealth implementation specialist today.